
Better screening can help GPs recognise anxiety disorders earlier
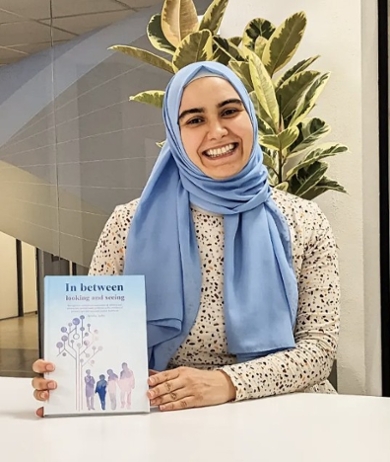
Only one in five young people with emotional health problems such as an anxiety disorder receives appropriate professional help. GPs often fail to properly recognise the signals in children and young people, according to psychologist Semiha Aydin. How can we improve this? PhD defence 23 February.
GPs regularly see children in their surgeries who have stomach ache or sleep issues, but these complaints can often be symptoms of a very different problem. Aydin: ‘It isn’t easy for parents and GPs to assess the seriousness of psychosocial problems. This is especially true for anxiety disorders because they are less pronounced than, say, hyperactive, problem behaviour.’ In her dissertation, Aydin focuses on the role of GPs. ‘With a calm, quiet child, people quickly conclude that this kind of introvert behaviour is part of their personality, but there are some children for whom there is more going on, and there could be an underlying social anxiety disorder, for example: they are so afraid of social situations, such as taking part in group activities, that they do all they can to avoid such situations.’
‘Often, anxiety symptoms develop first, and then other issues such as school dropout, mood problems or substance abuse.’
Anxiety disorders inhibit development
An anxiety disorder has a major influence on a person’s development, which can cause numerous other problems later on. Previous research has shown that three-quarters of adults with mental health problems already had symptoms before the age of fourteen. Aydin: ‘Often, anxiety symptoms develop first, followed by a range of other issues such as school dropout, mood problems or substance abuse as a means of suppressing the problem. This is why it’s so important to recognise anxiety disorders in good time.’ But, to be able to do that, we need more knowledge, she stresses: if GPs know that anxiety disorders are so common, they will be more alert to them. It goes without saying that a good talk with the child themself is essential. ‘As well as open questions like “How are things at school?”, it’s better to ask things like “Do you have friends?” and “What do you do in your free time?”’
Studies on GP assessments
Aydin carried out three studies. She presented a group of 229 GPs with descriptions of young people coming for a consultation, and for validation she gave the same descriptions to a small group of mental health professionals. The GPs recognised fewer potential anxiety disorders: on average in 1 in 8 of cases, compared with 5 in 8 by the mental health professionals.
In a second study, Aydin examined 723 mental health referral letters from GPs to LUMC Curium, a center for child and adolescent psychiatry. Aydin: ‘Some clinicians assume that referral letters are just another piece of bureaucratic red tape, but this study shows that we need to take the GPs and their referral letters more seriously.’ The letters contain a lot of useful information about the patient, the nature of the complaints and, for example, the family context, because the GP also knows the family. ‘This is one of the strengths of the GP. Continuing education and closer knowledge of symptoms are important to be able to recognise the signs better. In a quarter of the letters, children were referred because of possible depression, while they actually needed to be treated for anxiety.’
‘There are around 670 questionnaires. GPs often can’t see the wood for the trees.’
Jungle of questionnaires
The third study looked at questionnaires for diagnosing disorders. ‘There are around 670 lists that are portrayed as scientifically founded. This huge number means that GPs often can’t see the wood for the trees. Only four of all these questionnaires meet essential criteria such as containing well-balanced questions, and being free and user-friendly.’ One of them is the SDQ, the Strengths and Difficulties Questionnaire. Aydin advocates that GPs should use this questionnaire more often. The list contains 25 questions that parents and teachers can fill in. ‘This list allows GPs to be more certain of the child's mental state and helps them assess more quickly whether a referral is needed.’
Better cooperation between GPs and mental healthcare
Mental healthcare professionals can then make a more extensive assessment using the Development and Well-Being Assessment (DAWBA) that is linked to the SDQ. Using both lists avoids unneccessary repetition, and information van different informants - young people, parents and, for example, teachers - is properly combined, says Aydin. The questionnaires are also in line with what is needed in GP care and subsequently in mental healthcare. ‘GPs sometimes have the idea that clients aren’t keen on filing in questionnaires, but that’s mainly when nothing is done with them, and when every institution they approach wants something different.’
